
Extract Article Below: https://www.complexneedscapable.org.au/recognising-cognitive-impairment.html#indicators
Recognising cognitive impairment
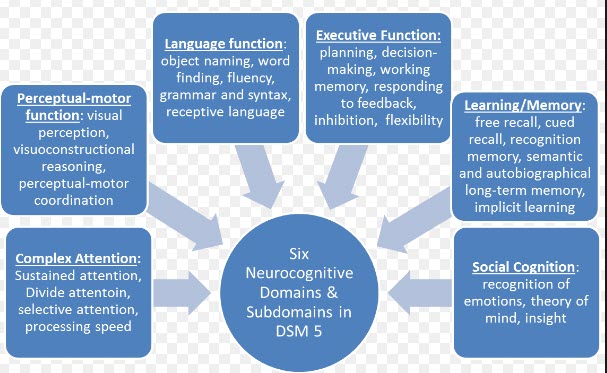
There are several domains of cognitive functioning, such as attention and memory, and each of these can be selectively or jointly impaired.
What is cognitive impairment?
Cognitive functioning or cognition refers to the processing of information by the brain, and can be described as a person's ability to think, concentrate, formulate ideas, reason and remember (Gray, Forell & Clarke 2009).
There are several domains of cognitive functioning, including:
- Attention
- Memory
- Visuo-spatial skills (which allow us to visually perceive objects and the spatial relationships among them), and
- Executive functioning (which includes tasks that help people learn new information, remember and retrieve information, plan, make decisions, and use information to solve problems).
Each of these domains can be selectively or jointly impaired across a range of developmental, neurological, acquired brain injury, mental illness, substance-related or dementia conditions. The term 'cognitive impairment' is used to recognise a broad range of disorders that affect cognitive functioning. Cognitive impairment may be 'hidden' from a worker when a person first enters a program, especially if the person has a mild impairment. Common causes of cognitive impairment are listed in the following table.
Common causes
| Developmental | Fetal alcohol syndrome and related disorders
Learning disorder Attention deficit hyperactivity disorder Autistic disorder/Asperger's disorder Intellectual disability |
| Acquired brain injury | Traumatic brain injury
Stroke Hypoxic brain injury Alcohol and other drug-related brain injury |
| Neurological | Multiple sclerosis
Huntington's disease Parkinson's disease |
| Mental illness | Depression/anxiety
Psychosis/schizophrenia |
| Dementia | Alzheimer's dementia
Vascular dementia Fronto-temporal dementia |
Common indicators
The indicators of a person with cognitive impairment are highly varied. They may have difficulties engaging with other people or services, identifying and maintaining suitable work or study, driving a car, carrying out daily activities (e.g. paying bills) or managing basic aspects of self-care. Cognitive impairment rarely occurs in isolation, i.e. without affecting both emotional and behavioural functioning. In fact, behavioural and emotional disturbances often reveal the presence of cognitive impairment.
Addressing cognitive impairment through compensatory or remedial approaches may reduce challenging behaviour and emotional distress. Some people lack the knowledge or resources to cope with their cognitive, behavioural and/or emotional difficulties and use alcohol or other drugs to cope, which often further impairs functioning in these domains. All three factors - cognition (thinking), behaviour (acting) and emotions (feeling) - affect a person's ability to get by in the world.
Neuropsychological Cognitive Behavioural Model

Source: Adapted from Berry (2012).
At a broad level, people with cognitive impairment will experience difficulties with adaptive behaviours. These include social, conceptual and practical skills they have learned in order to function in their daily lives (The Arc 2011).
A person with impaired conceptual skills, for example, receptive and expressive language, reading and writing, money concepts and self-direction may present with:
- A low literacy level
- Comprehension difficulties, including with abstract concepts and complex instructions
- Problems planning and organising daily activities
- Problems with budgeting and managing money.
A person with impaired social skills, for example, relating to other people and the external social environment, as well as self-esteem, personal sense of responsibility may:
- Have difficulties following rules (including laws)
- Respond inappropriately in some social settings
- Have low self-esteem
- Be vulnerable to victimisation.
A person with impaired practical skills, for example, personal daily activities such as eating, dressing and mobility may have difficulties with:
- Preparing meals
- Using transport
- Using the telephone
- Maintaining a safe living environment.
Hiding, masking or denying disability
Cognitive impairment is often masked. For most people who come into contact with drug and alcohol services, their cognitive impairment is in no way visible. It's only through observing their behaviour in the assessment process or while they're receiving treatment that we may get clues that they may have a cognitive impairment.
Many people with cognitive impairment are very good at hiding their disability. This may be because they want to fit in with everyone else or because they might be very high functioning in some areas of their lives or have very good expressive communication yet have very poor receptive communication. Also, people will have typically experienced discrimination, shame and humiliation as a consequence of being labelled due to their disability. Often if a person is aware they have a cognitive impairment, they won't readily admit to it.
AASGAA strongly recommends the following site from headway in the UK which explains functioning and brain damage. Extract below:
Neuropsychological Reports are very important BUT the results should always be seen by a Neuropsychiatrist or Neurologist as often we have seen Psychologist attempt to draw inferences from their own reports which are subsequently dismissed by Neurologists.
Assessments must focus on three areas:
Cognitive Testing
Behavioural Functioning
Physical Functioning
(Many Psychologists have ignored behavioural issues so be aware)
A Neuropsychological reports will look at the following areas:
Cognitive Functioning (Noting Behavioural & Physical Issues as well)
Cognitive functioning or cognition simply means information processing. There are many cognitive functions of the human brain, including:
Attention, including:
- Focused (or selective) attention
- Sustained attention (concentration)
- Spatial attention
- Attention span
- Divided attention
Memory, including:
- Verbal memory
- Visual memory
- Encoding
- Storage
- Retrieval
Language, including:
- Expression
- Comprehension
Visuo-Spatial skills, including:
- Visual perception
- Construction
Executive Functions, including:
- Idea generation
- Initiation
- Planning
- Reasoning
- Problem-solving
- Flexibility
The areas of affecting judgement and decision making are IQ (understanding), Reasoning and Memory Impairments (Recall and Retain). Cognitive flexibility is also an issue that needs to be addressed.
Clock drawing impairments and recall of information are areas to watch out for as the inability to plan is a sign of planning issues and making decisions.
Also note severely impaired attention can have a profound affect on other areas which will affect decision making. The whole brain and functioning need to be assessed to determine if a certain area of impairment is affecting the social and physical functioning of an individual.
It is possible to have only one severely impaired cognitive domain that will have a profound affect on other areas, even thought those areas are not primarily impaired.
Always ask: do these impairments affect decision making?
The whole functioning (Social and physical) must be factored.
Often physical and language impairments have been used to justify a lack of decision-making capacity. If these impairments are NOT affecting reasoning or decision making then the individual has capacity to make their own decisions.
On the other hand, if an impairment affects judgement like frontal lobe damage, then the ability to reason is impaired and a Neurologist will then have to determine the extent the impairment is affecting judgement, IQ and day to day ‘mental’ functioning. Minor damage in these areas can lead to chaos. Delusions, inflexibility, isolation and personality changes. Even if the individual ‘looks ok’.
Daily activities (washing, showering etc) are basic functions and not ‘higher’ level functions and do not confuse daily activities with higher level decision making (executive impairment).
Executive Impairment is the higher order decision making. The brains ability to co ordinate all the cognitive functions. Cognitive functions are the individual domains.
Executive Functioning is the most vital domain that affects decision making. This is the area one needs answered as well as memory impairments. Please click on links below for more details.
COGNITIVE DOMAINS ASSESSED
COGNITIVE ASSESSMENT FOR CLINICIANS
C M Kipps, J R Hodges
Neuropsychological Assessment - Step by Step
Cognitive screening and assessment
Cognitive screening and assessment
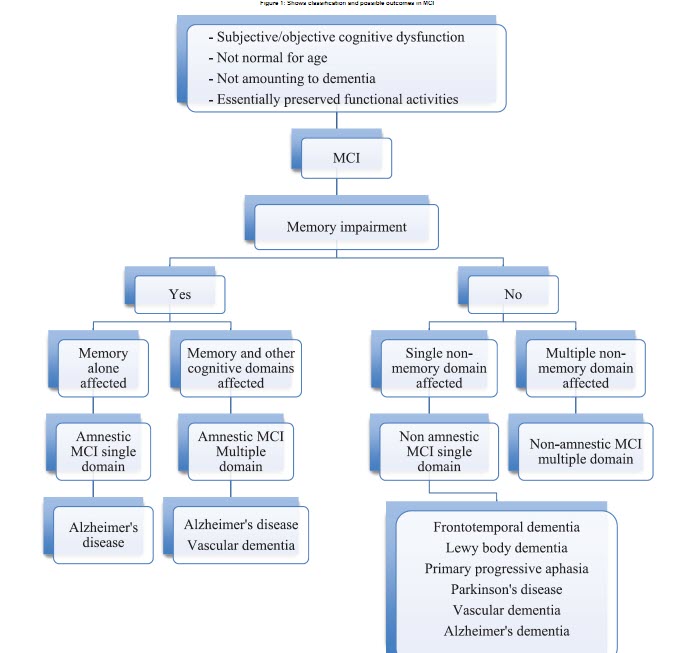
Why is an assessment for cognitive impairment and dementia so important? It is because an early diagnosis means early access to support, information and medication.
There is no single definitive test for diagnosing dementia. Assessment will account for behavioural, functional and psychosocial changes, together with radiological and laboratory tests. The assessment process may take three to six months to achieve.
Assessment:
Assess cognition if you have any indication or suspicion of impairment in your patient. This is the first step in determining whether or not your patient needs further evaluation.
DSM-5 definition and warning signs.
Take note of the history regarding cognition and function from informant:
It is important to take notes about the history of the patient from an "informant". An informant is someone who knows the patient well and has observed their cognition and function over time, for instance, a family member or close friend.
You could ask the 'informant' about the following in relation to your patient:
- Risk factors - vascular disease (link to our diabetes guide), alcohol, head injury, mood disorders, behavioural and psychological symptoms, recent illness, medications
- Activities of Daily Living (ADL), instrumental ADLs, cognitive complaints, mood, driving, safety
- Information from carer, family regarding changes and functional decline (time course = onset, progression)
Informant tools:
The following cognitive assessment tests are the most commonly used; however, it is important to choose the tests most suitable for your patient and for the health setting within which you work.
The General Practitioner assessment of Cognition (GPCOG)
A reliable, valid and efficient instrument for general practitioners to screen for dementia in Australian primary care settings.
The GPCOG involves two parts: a cognitive test for the patient and, if the result is uncertain, a short interview with an informant. The cognitive test takes less than four minutes to administer and includes the clock drawing test.
Research indicates that it as effective as the MMSE in primary care settings. The GPCOG is free.
Mini-Mental State Examination (MMSE)
This test is currently the most widely used cognitive assessment tool. It takes 10-15 minutes to administer. It is scored out of 30, with a score below 24 suggesting dementia.
It is used to assess global cognitive status. It is recommended for use in Acute, Primary, Community and Residential Care.
If used, the clock drawing test should be used as a supplementary test of frontal abilities. This is scored separately to MMSE.
Clock Drawing Test
This test involves asking patients to draw a clock on a blank piece of paper with the time set at 10 minutes past 11, or a variety of other suggested timeframes. A variety of scoring systems exist, but the simplest way is to rate the numbers as well planned or spaced and whether the hands indicate the right time. It can be scored as either normal (correctly drawn) or abnormal (any other result).
It evaluates organisation and planning. It is a useful screen for frontal functions of planning and conceptualisation.
The Rowland Universal Dementia Assessment Scale (RUDAS)
The Rowland Universal Dementia Awareness Scale is a short cognitive screening tool, recommended for use with those from culturally and linguistically diverse backgrounds.
Kimberly Indigenous Cognitive Assessment (KICA)
The only validated dementia assessment tool for older indigenous Australians.
For more information, please visit the Dementia Outcomes Measurement Suite, a Commonwealth Government initiative to assist health professionals in assessing dementia in all settings.
This website has assessment tools, manuals and scoring guides for download.
Opportunities for Cognitive Screening in General Practice
There are several opportunities in the practice to screen your patients for possible cognitive impairment and dementia. These include:
-
The 45+ Health Check
- An opportunity to pick up younger onset dementia in your patients under 65 years of age
- Build in questions about cognitive function, concerns about memory, mood and behaviour
- Look at possible risk factors for dementia (modifiable and non-modifiable in your patient)
- Can be charged to MBS item #717
-
The 75+ Health Check
- An opportunity to pick up possible cognitive impairment and dementia in your patient
- Modify the existing 75+ Health Check and include questions about cognitive function, memory, frailty, dexterity, driving and advanced care planning
- Can be charged to MBS item #705
-
The Chronic Disease Management/ Plan
- An opportunity to screen for possible cognitive impairment - in your patients under 65 years of age as well as over 75 years of age- undertake annually or bi-annually
- Can be charged to MBS item #721 (development of plan), #732 (review of plan), #723 (a Team Care Arrangement) , #731 (a plan developed for patients in residential aged care) and #10997 (practice nurse monitoring and support as part of plan)
-
Mental Health Treatment Plan (MHTP)
- An opportunity to be mindful of a possible diagnosis of dementia/cognitive impairment when preparing and reviewing a MHTP for your patient
- N.B. Dementia is not classified as a mental health disorder under the Better Access to Mental Health Scheme (hence, MBS items cannot be charged)
For more information:
Please visit the Medicare website
For training and advice on how to 'build dementia practice in your practice', please go to this section on online training.
IMPORTANT NOTES:
- If uncertain or inconclusive, repeat tests over time
- Use sensitive language when introducing the tests/assessment process to your patients and their families/carers
- Be prepared for questions from your patient or their families and carers; for example:
- What tests will be conducted?
- Who will be performing the tests and how long will it take?
- Should I prepare for the tests in any way?
- Will any of the tests involve pain or discomfort?
- Will there be any cost involved?
- What follow-up will be necessary and who will follow up?
- How will I be informed of the test results and the diagnosis?
Other diagnostic tests:
Mental state and physical examination
- Differential diagnosis - Look for specific conditions that mimic dementia (Depression - for example), Delirium (for example CAM) and Drugs/dosing interactions) or that can exacerbate dementia: for example cardiac failure, use of anticholinergic drugs
- Check nutrition, hygiene, visual or hearing impairment
Blood, urine tests and imaging
- Urinary tract and other infections
- Renal and liver (hepatic) function
- Rule out rare but reversible causes for example abnormal thyroid function, calcium or Vitamin B12 deficiency, electrolyte balance (salt and water), tumour
The following investigations are usual practice: FBE, EUC, LFTs, Ca, TFT, B12, Folate, MSU, ECG, and if indicated - VDRL, CXR, HIV
Imaging recommended include: CT brain, MRI, and if indicated - PET, SPECT, FRMI
For more information:
- Tests used in diagnosing dementia

(Dementia Australia help sheet Q&A 10)
- 14 essentials of good dementia practice in general practice
- Diagnostic criteria for dementia

(Dementia Australia help sheet Q&A 11)
Assessment of Behaviour and Psychological Symptoms of Dementia (BPSD)
Almost all patients with dementia experience BPSD; these are also referred to as neuropsychiatric, non-cognitive symptoms. The symptoms vary between patients and over time and can include:
- Mood disturbances (anxiety, apathy, depression, euphoria)
- Hyperactivity-type symptoms (aberrant motor behaviour, aggression, agitation, disinhibition, irritability, restlessness)
- Psychotic symptoms (delusions, hallucinations, paranoia)
- Other behavioural symptoms (changes in appetite, hoarding, night-time behaviour disturbances, wandering)
These symptoms become more common as the dementia progresses and present a major cause of stress to carers.
When BPSD occur, assess factors that may cause, aggravate or reduce the behaviour. Assessment should first exclude physical causes, such as delirium (common in patients with dementia), urinary tract infections or a drug interaction. Other factors, such as the environment and behaviours of others, should also be considered.
The assessment should ideally consider:
- Frequency of behaviour over time
- Context and consequences of the behaviour
- Mental health
- Physical health
- Medication side effects
- Previous habits and beliefs
- Psychosocial factors
- Factors in physical environment
- Possible undetected pain or discomfort
For more information about BPSD assessment and clinical support services for your patients, please go to the dbmas website or phone their national 24-hour helpline on 1800 699 799.
DBMAS provides 24-hour advice, assessment, education, intervention and specialised support to carers and care workers who provide support for people with dementia with moderate to severe behaviours of concern.
MEMORY & TYPES OF ILLNESSES
BEHAVIOURAL ISSUES
We have seen people with perfect Orientation, Language Skills and NO Memory issues assessed as having a Dementia. Sometimes this is due to pure Frontal Lobe Damage in the Frontal and Orbital area. AASGAA members have explained this a dealing with a 'stranger'.
Often Doctors focus on 'cognitive' ignoring behavioural issues. This area must also be assessed. Usually those closest to loved one can provide information and changes.
Behavioural changes often lead to breakdown in family relations and the person in question very vulnerable to abuse, exploitation and neglect.
Dementia: behavioural and psychological symptoms
The term dementia refers to a group of conditions that cause a progressive widespread decline in brain function. There are 4 main types of dementia, of which the most common is Alzheimer's disease.
What are the behavioural and psychological symptoms?
Loss of memory and intellectual function are frequent symptoms, but dementia can also cause changes in behaviour and mood. In fact, at least 90 per cent of people with the disorder will develop behavioural and psychological symptoms of dementia (BPSD).
Some examples of BPSD are:
- repetitive behaviour;
- mood disturbance (e.g. depression);
- social inappropriateness;
- agitation;
- wandering;
- psychosis, which may include delusions (false beliefs) and hallucinations (seeing or hearing things that are not actually there);
- physical aggression; and
- sleep disturbance.
Why do these symptoms occur?
BPSD can be due to a number of different causes. Some of these symptoms are part of the underlying dementing process, but it is important to try to determine if any other factors might be contributing.
If carers notice a change in behaviour of a person with dementia, they should discuss it with their doctor. The doctor will be able to assess whether the person may be suffering from a psychological disorder such as depression.
They will also be able to assess whether an underlying physical disorder has brought about the change in behaviour, for example, physical discomfort due to ongoing constipation or urinary incontinence.
How can these symptoms be managed?
Behavioural symptoms can often be quite challenging to cope with for carers of people with dementia.
Carers should discuss with the doctor ways in which they can best help manage these symptoms. Some simple examples of this may include:
- maintaining a familiar environment;
- large face clocks, calendars and signs to improve orientation;
- providing pleasant stimulating activities;
- encouraging exercise and group activities;
- following set routines for daily tasks; and
- providing a calm clear explanation about any changes to the routine.
Alzheimer's Australia also provides information regarding behavioural changes in dementia and offers education and support for carers. These behaviours can be very stressful for those dealing with them.
If a person with dementia is found to have depression, antidepressant medicines can be effective. There is also some evidence that medications called cholinesterase inhibitors may decrease the development of behavioural disturbances in Alzheimer's disease.
Other medicines may be helpful for symptoms such as agitation and aggression or for psychotic symptoms, but these need to be used with caution because of side effects. They are therefore usually only used in severe cases, when immediate treatment is needed or when other attempts at management have failed.
TICK LIST
